Beating the Odds – A PPROM Story
It sounds so easy to do: just stay pregnant. Every minute and every single hour that I could stay
pregnant gave my daughter a better chance of thriving after birth.
My life changed forever in January 2016. I was happily pregnant and getting into the routine that
every nesting mother-to-be does. My registries were done and the maternity photos scheduled, along
with all plans for the pregnancy and birth. We met with pediatricians and chose one; we met with a
doula and started planning our birthing experience. My birth plan was “to make it out alive”, and
looking back on it I wonder if subconsciously I knew my pregnancy was about to become a crisis.
My water broke unexpectedly when I was 27 weeks and four days pregnant. I awoke to find my pants
wet and thought it was urinary incontinence. As I got to the bathroom, I realized my worst fear was
happening. I sat completely still and listened to the sound of fluid leaving my body. From that
moment on I knew my life would be different. I yelled to my husband who was still asleep in bed:
“Dave, I think my water broke?!” Completely puzzled, we called the OBGYN who directed us to go to
the hospital. We made it to the hospital and were greeted by a girl I had known from school. She
placed me in a wheelchair and took me to Labor & Delivery. By the look of devastation on her face, I
knew I wasn’t going home.
 In Labor & Delivery, the staff checked and tested my discharge to
In Labor & Delivery, the staff checked and tested my discharge to
determine if it was amniotic fluid. I was diagnosed with PPROM
(Preterm Premature Rupture of Membranes), which affects 150,000
women in the US every year. It is the leading cause of premature
birth and can result in serious and life-threatening complications for
both mom and baby. I was immediately given a steroid shot to help
develop my daughter’s lungs followed by a magnesium drip, which
has terrible side effects but helps stop labor and works to prevent
brain bleeds in premature babies. Since I wasn’t dilated or
contracting, I was taken by ambulance to a hospital with a higher
level of care to accommodate my daughter and I. If my daughter
had been born at the first hospital, the staff would not have been
able to resuscitate, because they were not able to handle a baby at
that gestational age.
“We would have lost her in moments.”
After arriving at the second hospital, I endured hours of testing and ultrasounds. I was deemed stable
and transferred to a Maternal Special Care Unit, which is a step-down intensive care unit for
pregnant women. The plan was to stay pregnant until 34 weeks while admitted to the hospital. That
meant no baby shower, no maternity photos, and spending my entire third trimester in the hospital.
With all of this lost in a matter of moments, I was fortunate to still be pregnant. Every single hour
counted, and every minute that I could stay pregnant meant a better possibility of a positive outcome.
The next few days were filled with constant fetal monitoring, IVs, and ultrasounds. We were told the
NICU would send someone to talk with us about what to expect. Those weeks were a roller coaster of
emotions. What would happen to my baby and I? Could I stay pregnant for another seven weeks? Why
did this happen to us?
Hours folded into days, and we were comfortable and in a routine. My husband stayed by my side for
the entire duration. We were in this together. The room had a pretty view of the water. Family
members sent bouquets of beautiful flowers to help brighten our room. We had a few visitors, but it
was difficult to hear people call our hospital stay a “vacation”, even though they were joking. Fighting
for your life while hoping to save the life of your unborn child is not a vacation.
“Every moment that I could stay pregnant mattered…”
I was fortunate to be surrounded by nurses that were extraordinary. Our favorite nurse was Kate. She
held me as I cried hysterically one night. She hugged me, mother to mother; she recognized that I was
working so hard to stay pregnant. Kate understood and validated me. She held me for what seemed
like forever; Kate assured me it would be okay and that we would make it out on the brighter side.
Kate had a heart of genuine gold. To this day I’ve done my best to relay how much that moment
meant to me, and to my husband as well. The other nurses were great too. They shared stories of their
kids and how their days were going. They made me feel like one of their own. I felt special and
supported in this situation because they truly understood what we were experiencing. My nurses will
forever hold a special place in my heart.
I often asked the nurses what typically happens when someone has PPROM. They stated the goal was
to make it to 34 weeks. The nurses remained optimistic that I would be in good hands no matter what
kind of situation arose. Each day my goal was to reach the next day while remaining pregnant.
At 29 weeks and one day, I was in labor. I woke up around 3:00 a.m. with contractions and they were
getting stronger. My nurse Sam hooked me up to monitoring and gave fluids to see if that could
potentially stop the contractions, but it wasn’t working. Sam called in one of the doctors and they
examined me, but I was only one centimeter dilated. My contractions weren’t registering on the
monitors. After a few intense contractions, the staff brought me down to Labor & Delivery. By 8:30am I
had an IV line replaced and an ultrasound done. I consented to a C-section, and was given oxygen
and morphine to stop the pain from contractions.
When the next round of doctors came by, things quickly reached crisis level. After a quick evaluation,
the doctor realized that my daughter had a prolapsed cord and my placenta was abrupting. The
doctor screamed “cord!”, and the anesthesiologist jumped on my bed while I was quickly wheeled to
the Operating Room. I screamed for my husband, but there wasn’t enough time for him to reach us. It
was chaos, and I was terrified. Just as they were getting ready to put me under, a gentle face with
glasses popped over and put his hand on my forehead. My doctor said, “Let’s do this! Let’s get her
here, okay?” Within minutes our daughter was born, crying and breathing on her own. From what I was
told there wasn’t a dry eye in the operating room.
Staring at my daughter in her isolette in the NICU
just hours after birth was surreal. I was delirious from
pain medication and couldn’t comprehend the
magnitude of the situation. I watched her tiny chest
rise up and down while I sat by her side in a
wheelchair. I only wanted to hold her and feel her for
the first time. Doctors and nurses tried to explain
what happened in the hours since birth and
discussed the care plan for “baby girl Devino”. She
came so early that we had not yet chosen a name.
Days later my husband and I decided on a name with
meaning; we chose Julia Grace, which means
“youthful” and “of God”.
I spent hours pumping so my husband could transport
my milk to the NICU. All I could do was pump and
pray. The next 50 days were filled with learning a
whole new language: grams, ML’s, CPAP, sodium,
TPN, and so on. The nurses in the NICU became our
family, they were instrumental to our success. They
celebrated even the smallest gains with us and
encouraged us when we were overwhelmed. We
experienced so many “firsts” in the NICU: Julia’s first
bath, her first bottle, and many other milestones.
I held my daughter for the first time two whole days after she was born, on February 8, 2016. I had a
nurse help me sit next to the isolette while my husband assisted with the wires and tubes attached
to our little girl. She was so fragile to me, but she was strong. I watched my husband’s eyes fill with
tears as he sat in our little space next her isolette. I sobbed that I couldn’t wait to meet her and that
I was sorry that I couldn’t keep her safe. I was finally able to feel her skin against my chest and feel
her breathing. I will never forget that moment.
Those were the most emotional days of our lives. My entire purpose for living was a preemie baby
weighing a mere two pounds and four ounces. She was incredibly feisty. Reality quickly set in for us,
as I would be discharged without our baby. I was leaving a piece of my heart behind. We were just
beginning a very long and emotionally-charged journey to bring Julia home. After being discharged I
had a few very close friends come visit me at home. They helped set up her bedroom, kept me
company, and were encouraging and loving. Our friends and family brought us food and even my
favorite coffee. They let me know that they were there for the three of us. We needed their support
more than ever to encourage us and to bring a sense of normalcy to the situation.
“My husband and I both missed her birth.”
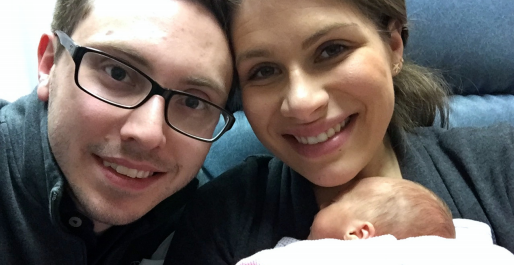 My husband had returned
My husband had returned
to work, and I was home
alone. I was a wreck, but
continued to pump
and we would visit our
little girl in the NICU. I
began to struggle with
Post-Traumatic Stress
Disorder and Post-Partum
Depression, which are
extremely common for
preemie parents following
a traumatic birth
experience.
Twenty months later I am finally recognizing that I need help to make myself feel better, and help to
find the person who I was before everything changed. I knew that no matter what happened that
morning, we had a care team that reacted swiftly to make sure we survived. In the weeks following my
delivery, I tracked down people who were in the operating room. I wanted to hear what happened at
Julia’s birth. Though my husband and I both missed her birth, I am happy that the doctors and nurses
jumped to action that morning because my husband would have lost both of us. I would later invite
them to meet Julia and take a picture with her before we left to go home, one small way of telling her
story. My favorite was the delivering doctor, who gave her the sweetest kiss on the cheek and
snuggled close for a picture.
I often think that I don’t acknowledge my husbands’ role in my recovery enough. He’s seen me fall
apart and pick myself back up. But I never had to do this alone; he has always been right there
beside me. He held me when I was sick, encouraged me to pump, helped me understand the
positive impact pumping had, pushed me in a wheelchair see our daughter, and was my best friend.
He helped me find the silver lining and kept the focus on our little family. Maybe this was a way for
us to take a step back from the roles we played and for once be selfish with our time and love. We
were completely devoted to the care of our daughter. We were both changed because of our
PPROM and NICU experience.
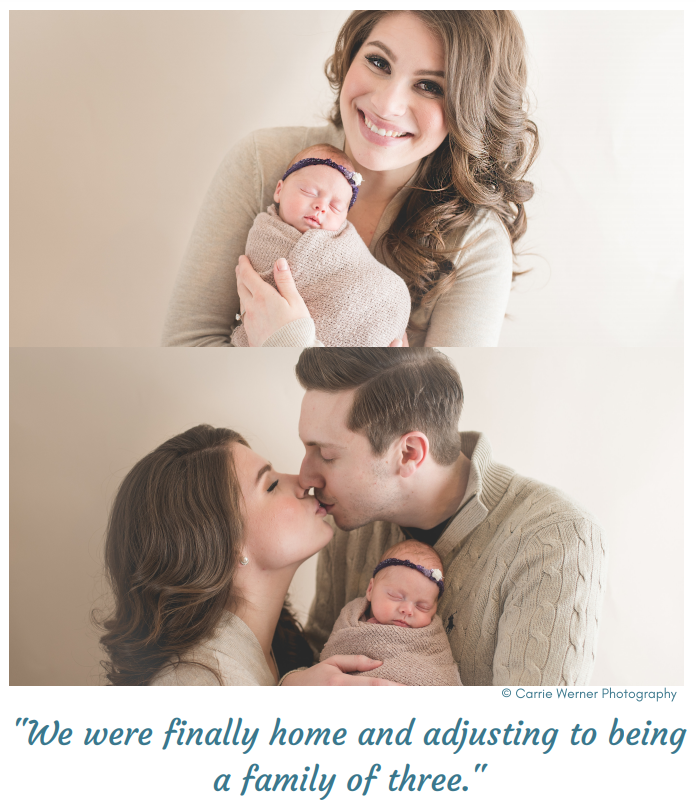
We happily brought Julia home after 50 days in the NICU on Easter Sunday. We remained in
isolation for the first month she was home, until she reached 40 weeks gestational age. and
we continue to be extremely cautious with visitors or others who have been sick. We weren’t able to
share our new bundle of love with family & friends immediately. Even though our first few weeks
were sleepless and a blur, I wouldn’t change it for the world.
I happily watch my daughter reach her milestones. It is surreal to me that such a happy and vibrant
little girl has endured most than more than most people will in their entire lives. It was so hard to
leave her every night for 50 days under the care of someone else. But throughout that journey we
met some amazing women who became our extended family. We are so thankful for our NICU family,
as they encouraged us to have faith that we would see the light at the end of the NICU tunnel. We
look forward to celebrating and sharing future milestones with the people entrusted with Julia’s care
while in the hospital.
Having a PPROM experience makes you appreciate the smaller things in life. Having a baby changes
you, but having a premature baby shakes you to your core. After my water broke at the end of the
second trimester, I was no longer the happily pregnant woman getting ready to welcome a bundle
of joy. My husband almost lost both of us the morning she was born. We’ve changed; we’re different.
I’m bitter and hardened, and sometimes emotionless in situations. I learned that self-care is
incredibly important. Take care of you, and put your emotional needs first. I was healing from an
emergency C-section while trying to come to terms with our experience. I saw my daughter through
the plastic walls of an incubator for nearly two months. Not a lot of people asked how my husband
and I were, and perhaps they didn’t know how to approach the topic. The pain from my PPROM
experience is still real. It’s hard to put into words the sense of loss that I feel. People sometimes say
that I missed the uncomfortable parts, but I feel much differently. I’d trade everything to have those
last 12 weeks of pregnancy back and reach full term.
“We beat the odds; we are PPROM survivors.”
This article was published on October 23, 2017 on The PPROM Foundation Facebook website, located at www.facebook.com/ppromsupport
“Support for when your water breaks, but your hope doesn’t”